
Integrating Social Care Delivery into the Opioid Epidemic Response
How addressing social drivers of health (SDOH) improves health outcomes for those affected by opioid use disorder (OUD).
It is estimated that more than six million Americans ages 12 or older have an opioid use disorder (OUD) and that in 2023 there were more than 110,000 drug-involved overdose deaths. The opioid crisis is a multifaceted challenge that requires a comprehensive approach, integrating both medical and social support systems, to shape the recovery journey of affected individuals. To effectively combat OUD, interventions must target the underlying social drivers of health, as factors such as economic hardship, housing instability, and limited access to mental health services can exacerbate both the prevalence and severity of OUD.
Risk factors associated with opioid use, misuse, and overdose include:
- Younger age – Drug overdoses and poisonings are the third-leading cause of pediatric deaths in the U.S.
- History of adverse childhood experiences (ACEs) – Analysis of Behavioral Risk Factor Surveillance System (BRFSS) data found that individuals reporting three or more ACEs had increased odds of taking opioids more than prescribed or without a prescription.
- Polysubstance use – More than 90% of individuals with OUD used more than two other substances within the same year and the majority of OUD-related deaths involve multiple substances.
- Other untreated mental health issues – Individuals with mental health disorders (e.g. anxiety, depression, bipolar).
Strategies for Addressing the Opioid Epidemic
Considerable progress has been made at the federal, state, and local levels in deploying evidence-based strategies to address the opioid epidemic. These strategies include primary prevention (e.g., reducing clinically inappropriate prescribing), harm reduction (e.g., Narcan distribution), evidence-based treatment (e.g., buprenorphine access), and recovery support (e.g., via peer support services). Ensuring equitable access to these essential interventions will undoubtedly prevent overdoses and save lives. The Centers for Disease Control (CDC) identifies that clinicians, community leaders, education, criminal justice, social services, business, and government all have a role to play in increasing access and linkage to care.
The CDC also recommends that linkage to care is bundled with other services (e.g., housing support, transportation assistance) to alleviate common barriers to treatment success, as effectively addressing the opioid crisis requires acknowledging and addressing the social drivers of health (SDOH) that contribute to OUD. By focusing on these underlying community-level factors — such as economic stability, education, healthcare access, and social support systems — we can create more comprehensive and sustainable solutions for the prevention and treatment of OUD.
Social Care and Opioid Use Disorder: Insights from the Literature
SDOH refers to the social, economic, and environmental factors that influence an individual’s overall health and well-being. Health-related social needs (HRSN) are the specific, actionable needs an individual may have within the broader social drivers of health. In recent years, a growing number of studies have emphasized the value of addressing the social needs of individuals with substance use disorder (SUD), defined as the inability to control the use of legal or illegal substances (such as stimulants, opioids, alcohol, or medications). Given the high rates of morbidity and mortality among individuals with OUD, along with the common occurrence of multi-substance use in this population, it’s unsurprising that many of these studies focus on individuals affected by OUD.
- A 2023 evaluation of California’s Whole Person Care Pilot – designed to coordinate the health, behavioral, and social care needs of Medi-Cal beneficiaries – found that participants with SUD experienced fewer ED visits ($32 per beneficiary per year decrease) and fewer hospitalizations per 1,000 beneficiaries ($310 per beneficiary per year decrease).
- A 2023 retrospective study to assess the impact of recovery housing for individuals with SUD found that providing housing helped reduce readmissions to inpatient substance use treatment and that housed individuals had reduced ED use and increased primary care use.
- A 2021 study funded by the National Institute of Drug Abuse found that case management, including service linkage to address basic needs, reduced inpatient readmissions and ED visits among a sample of 400 adults with comorbid SUD (including OUD)
- A 2020 study of a model that integrates maternity care, SUD treatment, and social service coordination for pregnant Medicaid beneficiaries with OUD found that participants experienced reductions in foster care placements, fewer reports of child maltreatment, and an increase in prenatal visits.
- A 2023 qualitative study to explore the perspectives of community-based clinicians and staff highlighted the need for better bidirectional care coordination between healthcare and community settings to support individuals with OUD. Participants reiterated that medication was important, but solving unmet social needs associated with ongoing opioid use was equally important. One clinician offering wrap-around support service stated: “They don’t know that services like ours exist. They think, ‘I can get meds, but how is that gonna help me with a place to sleep? Help me get my food stamps?’”
The Data is Clear. But Are Individuals in Need Getting Connected to Vital Services?
Most adults with SUD (94.7%) report not seeking treatment because they perceive that they do not need it. However, of the more than two million people with an unmet need for treatment, nearly half report that they do not know how or where to get treatment. Additionally, disparities in access to evidence-based treatment exist across groups. Based on an analysis of 2021 Medicaid claims data, one in three Medicaid enrollees with OUD did not receive medication-assisted treatment. Black/African American individuals, youth ages 18 years and younger, and individuals with a disability were all less likely to receive treatment.
Interventions that identify patients with SUD, initiate treatment, and link patients to community-based organizations (CBOs) are increasingly common, however, a 2023 scoping review identified several barriers to intervention success, including difficulties with:
- Building partnerships between hospital and community-based SUD programs
- Managing logistics and communication between hospital and community treatment teams to coordinate follow-up care for patients
Care in the clinical setting alone is not sufficient to address prevention, treatment, and recovery. Individuals with substance use disorders need clear access to comprehensive services such as employment, childcare, and housing. Building a path to recovery requires shared infrastructure to support community participation, coordinate care across service areas, and identify and activate evidence-based programs that effectively address diverse needs.
Insights from a Cross-Sector Collaboration Platform
Unite Us is an integrated suite of social care solutions designed to streamline processes and foster collaboration across government, healthcare, health plans, and community organizations to address SDOH. Insights from the Unite Us platform demonstrate how community-based organizations across the nation are collaborating to fight the opioid epidemic.
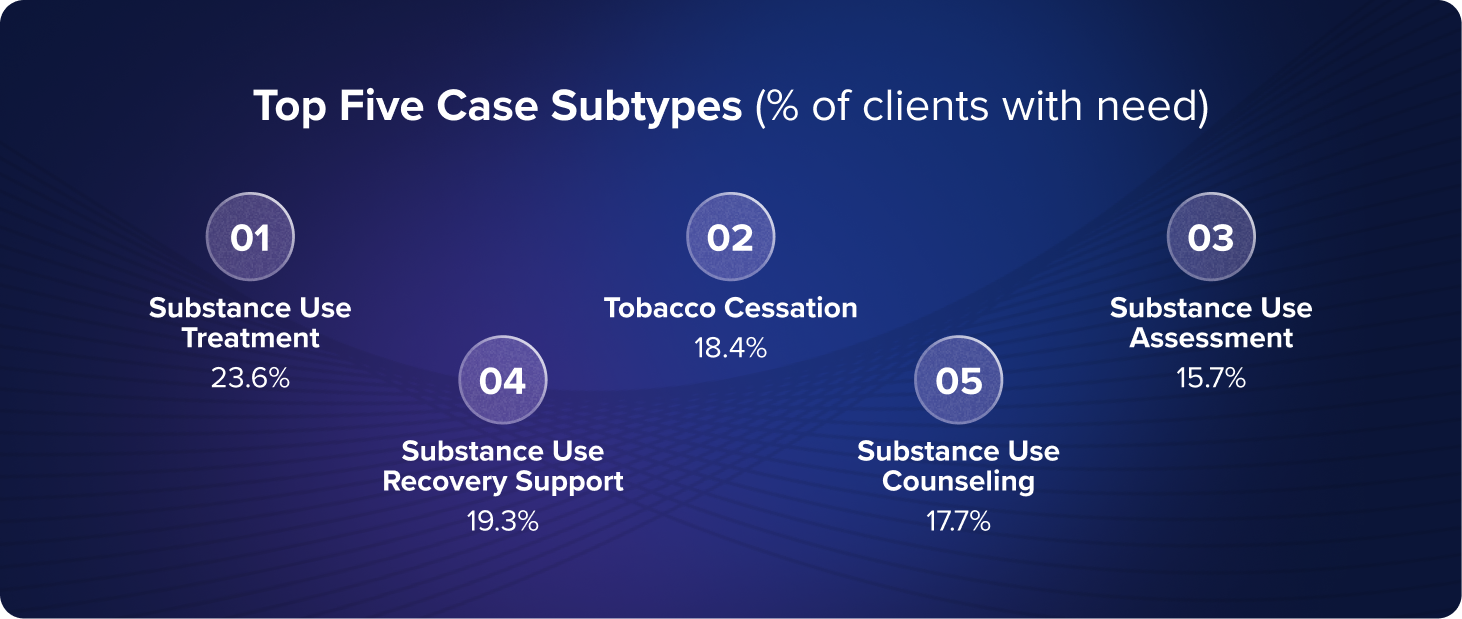
Since 2018, care professionals (e.g., community health workers, care coordinators, social workers) have leveraged Unite Us to connect more than 11,000 individuals with services to support their SUD recovery journey (15,000+ substance use cases). The top service subtypes referred to included substance use treatment, substance use recovery support, substance use counseling, substance use assessment, and tobacco cessation.
Data shows that substance use needs often co-occur with other types of needs. For example, nearly 1 in 4 individuals with a substance use need also had a mental and behavioral health need, one in 5 had a housing and shelter need such as transitional or emergency housing, 10% needed food assistance, and 10% needed support with benefits navigation (e.g., applying to health insurance). Effectively addressing the opioid epidemic requires recognizing that individuals with opioid use disorder may have co-occurring unmet HSRN that impact their ability to connect with ongoing treatment.
We observed an overall need resolution rate of 59% for substance use assistance requests, with no difference in resolution by gender, age, or military affiliation. However, we did find that the presence of co-occurring need requests can significantly influence the likelihood of substance use need resolution. For instance, the co-occurring presence of requests related to housing or shelter, food, and utility assistance, reduced the likelihood of resolution by 18%, 51%, and 40%, respectively. Conversely, needs related to individual and family support, mental and behavioral health, and transportation increased the likelihood of resolution by 158%, 50%, and 57%, respectively.
How Unite Us Ensures Privacy and Dignity of Individuals with SUD
Prioritizing the privacy and dignity of individuals seeking care is fundamental to the Unite Us mission. Individuals seeking care should trust that their information will be protected and secure. That’s why we protect social care information under the same strict security standards required for protected health information under HIPAA, applying heightened protections for sensitive information such as SUD treatment information.
Supporting Individuals with OUD: Where Do We Go from Here?
- Recognize that individuals with OUD may have co-occurring unmet health-related social needs that impact their ability to connect with affecting and ongoing treatment. When using validated tools to assess the presence of SUD, also consider assessing for unmet social needs (and vice versa).
- When designing and implementing interventions, consider the unique needs of specific populations, such as justice-involved individuals, pregnant and postpartum individuals, American Indians, and Alaska Natives. Include the voice of individuals with lived experience of substance use challenges to inform compassionate, practical, and responsive solutions to real-world barriers to recovery,
- Continue to deepen our understanding of how addressing social factors can improve outcomes for individuals with opioid use disorder (for example, how does access to stable transportation affect adherence to medication-assisted treatment? Or what combination of social services yields the best outcomes for individuals in OUD recovery?)



