Streamline Social Care Revenue Cycle Management and Measure Impact
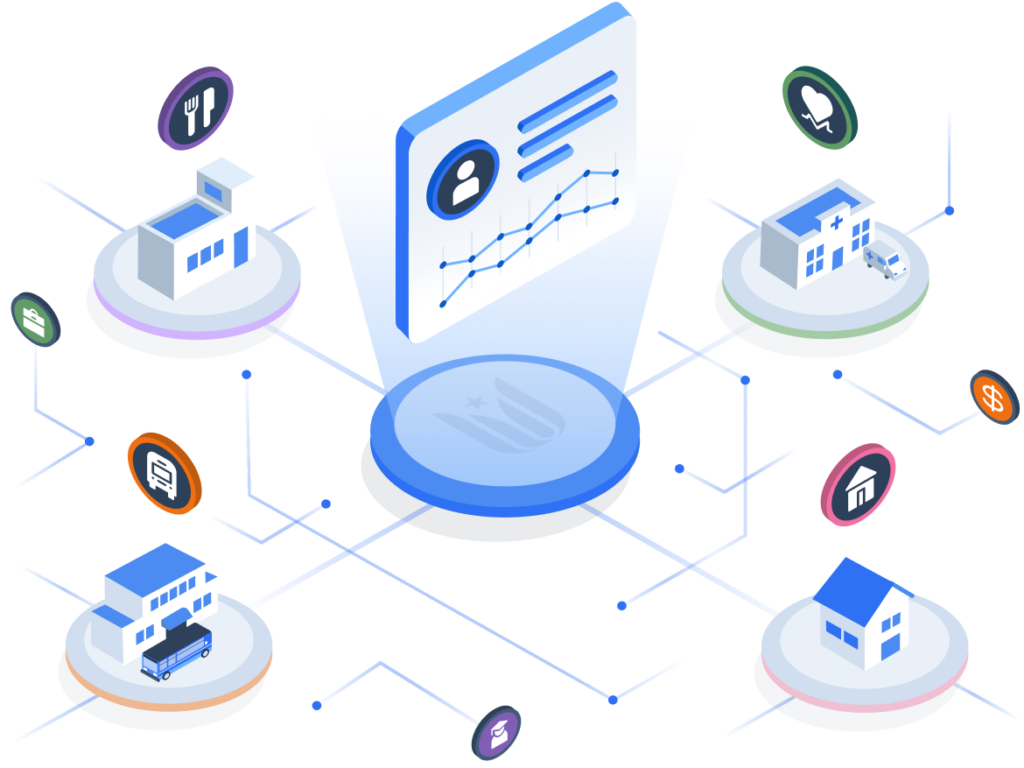
With Unite Us, spend more time serving your community and less time managing the back-end process.
Simplify and Scale Social
Care Reimbursement
Unite Us Social Care Revenue Cycle Management solutions simplify the complex landscape of social care reimbursements. We automate invoicing workflows to promote accurate, timely payments. With our robust reporting tools, you can manage payment workflows, reduce administrative burden, and minimize billing denials.
Why Partner with Unite Us for Social Care
Revenue Cycle Management?
We help you streamline processes, reduce billing errors, and gain actionable insights, so you can receive accurate and prompt reimbursement and demonstrate the impact of your work.

Streamline Social Care Reimbursement with Simplified Invoicing
Unite Us simplifies invoicing and claims for community-based organizations (CBOs). Our platform automatically pulls funder details, generates invoices and claims, and tracks billing statuses, enabling accurate and timely reimbursement. Our comprehensive documentation supports transparency and dispute resolution. By reducing administrative burden and minimizing errors, we help CBOs get paid faster.
Key Benefits
Streamline reimbursement and reduce errors
Enable transparency and quicker financial processing
Minimize delays and improve payment accuracy

Seamlessly Verify Coverage and Eligibility for Social Care Services
Verify coverage and eligibility for social care services in real time with Unite Us. Our platform eliminates the need to navigate multiple systems, streamlining the process of verifying eligibility and managed care enrollment. This not only reduces administrative burden but also minimizes billing denials, enabling smoother service delivery.
Key Benefits
Streamlined integration with health plans
Automatic and ongoing coverage verification
Faster case resolution
Lower claims rejection

Streamline Client Enrollment With Smart Workflows and Less Guesswork
Unite Us streamlines enrollment with flexible, tailored solutions. Users can complete standardized assessments for eligibility screening, and our Enrollment Workqueue centralizes request and assessment reviews. Customizable documentation creates a seamless process for staff and clients.
Key Benefits
Improve accuracy and reduce errors
Facilitate faster enrollment and access to services
Streamline workflows and reduce administrative complexity

Prove ROI of Social Care Investments with Payments Data & Dashboard
Unite Us offers powerful data reporting tools that help demonstrate ROI. Our Payments Data & Dashboard allows you to easily identify trends, measure performance, and demonstrate the financial impact of your programs. Whether evaluating funded services or showing value to stakeholders, our tools provide essential data-driven evidence for decision-making and sustainability.
Key Benefits
Track fund distribution across organizations, funding streams, and programs
Track billing revenue cycle for reimbursable services
Monitor real-time performance of CBOs

Unlock More Insights
Frequently Asked Questions:
-
Trust and transparency are the cornerstones of the Unite Us Platform. Unite Us is compliant with HIPAA and leading security frameworks including HITRUST. Read more about our security guidelines and our privacy policy.




-
Social care reimbursement is still relatively new, and managing the revenue cycle–from eligibility and authorization process to fee schedules and service codes–is incredibly complex. Unite Us takes the guesswork out of invoicing and reimbursement. As a result, our average claims denial rate is 1.56%—significantly lower than the industry average of 18%.
-
Our customers include health plans, state agencies, and CBOs across the country. We are proud to power HRSN reimbursement in Medicaid waiver states including North Carolina and Oregon.