
How Social Care Technology Improves Dental Access and Member Engagement in Connecticut
 The Connecticut Dental Health Partnership (CTDHP), serving more than one million Medicaid members, has significantly improved dental access through the implementation of the Unite Us closed-loop referral system. By leveraging real-time data and a high-touch service model, CTDHP increased dental service utilization among at-risk and underserved populations. This approach highlights the effectiveness of combining technology with personalized care to address barriers and improve oral health access for Medicaid beneficiaries.
The Connecticut Dental Health Partnership (CTDHP), serving more than one million Medicaid members, has significantly improved dental access through the implementation of the Unite Us closed-loop referral system. By leveraging real-time data and a high-touch service model, CTDHP increased dental service utilization among at-risk and underserved populations. This approach highlights the effectiveness of combining technology with personalized care to address barriers and improve oral health access for Medicaid beneficiaries.
Key Takeaways
In this report, you’ll learn:
Pathways to Oral Health: How Social Care Technology Improves Dental Access and Member Engagement in Connecticut
- Accurate Member Information Enhances Member Connections and Efficiency: Access to accurate and up-to-date member contact information within the Unite Us platform significantly enhances member outreach initiatives by enabling members to receive timely and right-sized navigation support.
- Staff Expertise Drives Stronger Referral Outcomes: CTDHP demonstrates strong proficiency and effectiveness in processing referrals within the platform, with a high acceptance rate, quick response times, and successful resolution.
 Platform Use Increases Dental Utilization: In 2023, of the members contacted by CTDHP staff from a Unite Us referral, 25% utilized dental services within 120 days of contact, of which 16% were for preventive dental visits. This is 11 percentage points higher than the average utilization rate from other CTDHP engagement campaigns.
Platform Use Increases Dental Utilization: In 2023, of the members contacted by CTDHP staff from a Unite Us referral, 25% utilized dental services within 120 days of contact, of which 16% were for preventive dental visits. This is 11 percentage points higher than the average utilization rate from other CTDHP engagement campaigns.
Background
The Connecticut Dental Health Partnership (CTDHP) is the contracted Dental Plan for Connecticut’s HUSKY Health Program, serving more than one million Medicaid members in the state. CTDHP aims to ensure all members have access to oral health services by meeting their acute needs, removing obstacles to care, and increasing members’ oral health literacy. This case study highlights the impact of this innovative approach on improving dental access for Medicaid members.
Each year, there are approximately 2.1 million emergency department (ED) visits for preventable dental conditions, costing the U.S. healthcare system over $2 billion annually.
Source: www.hcup-us.ahrq.gov/reports/statbriefs/sb280-Dental-ED-Visits-2018.pdf.
Challenge
While the rate of dental service use among Medicaid adults in Connecticut is one of the highest among all states, due in part to the state’s extensive Medicaid dental coverage policy, only 28% of continuously eligible adults and 61% of continuously eligible children utilized dental services in 2023.
One major challenge in improving access has been reaching and engaging members, as outdated contact information in state Medicaid eligibility files has often prevented them from connecting with members in a timely manner.

“The CTDHP Oral Health Navigation and Member Services teams are critical in reducing the barriers between Medicaid members and necessary dental care. Barriers to oral health care are complex and include access, oral health literacy, dental fear and anxiety, and social drivers of health.”
Kate Parker-Reilly, CTDHP Executive Director
Solution
To address these challenges, CTDHP implemented the Unite Us closed-loop referral system in 2022. Unite Us’ platform enables proactive outreach to members and warm hand-offs to community-based organizations (CBOs) that can help address barriers to care, helping all CTDHP members secure a dental home where they can receive routine, preventive care. The platform also facilitates real-time access to accurate and up-to-date member contact information.
- Member Services Representatives (MSRs): Receive the majority of inbound Unite Us referrals for members’ routine dental care needs, such as scheduling a routine appointment or identifying a dental home. MSRs receive an average of 6,000 phone calls per month from members, providers, and community partners and place more than 500 outbound calls per month.
- Oral Health Navigators (OHNs): Provide longitudinal care management to members with more complex care or accurate dental needs. OHNs work with an average of 500 members per year, with an average case length of 90 days. They address obstacles such as dental phobia, cognitive/developmental/behavioral challenges, barriers to treatment, and limitations in navigating the oral health delivery system.
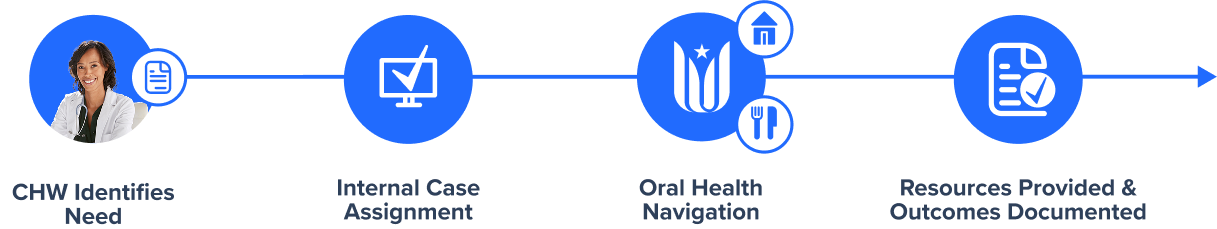
How it works
CTDHP collaborates with the Community Health Network of CT (CHN-CT), whose community health workers screen members for oral health needs and refer members in need to CTDHP via Unite Us.
Impact
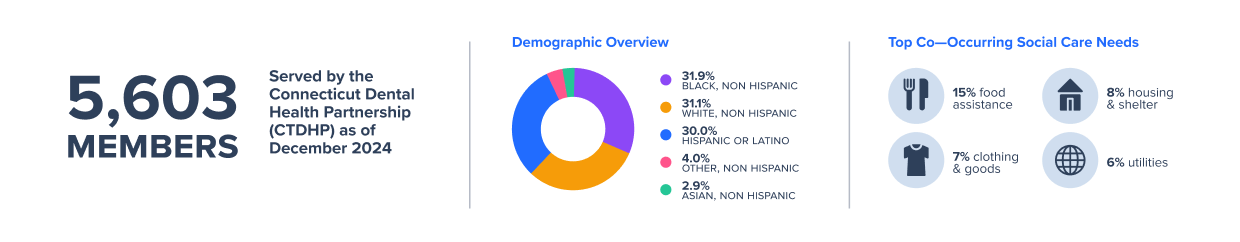
Since integrating the Unite Us closed-loop referral system, CTDHP has seen steady growth in member referrals for oral health services, managing 5,761 social care cases for 5,603 members by the end of 2024. On average, referrals were accepted in under one day, with 94.7% case resolution for Dental Care and 88.6% for Health Insurance/Benefits, and cases closed within a median of six to seven days, respectively. For cases closed as ‘Unresolved,’ the top reason was ‘Unable to Contact Member.’ In addition to the dental health referrals received, CTDHP sent more than 100 referrals to 49 community-based organizations, aiming to address non-medical needs identified for 45 members.
Technology’s Impact on Real-World Access and Engagement
In 2023, 25% of members contacted by CTDHP staff via a Unite Us referral utilized dental services within 120 days, with 16% of these visits being for preventive dental care. This is 11 percentage points higher than the average dental care rate from other CTDHP engagement campaigns. The high-touch service model has also increased trust and engagement among members, leading to better health outcomes and reduced barriers to care.
Lessons Learned from CTDHP Staff
In November 2024, three CTDHP oral health program staff members reflected on their experiences with implementing and utilizing Unite Us in their roles. Below are three key themes that emerged from their insights.
Personal Connection Builds Trust and Comfort with Members
- Encouraging Open Conversations About Social Needs: A social needs assessment is included in the intake process with a 30-item questionnaire, and conversations are encouraged during each encounter due to the evolving nature of social needs. OHNs and MSRs have the training and experience to build rapport and conduct the intake as a conversation in order to encourage honest responses from members.
- High Touch Service Increases Trust: When asked about members’ comfort level discussing social needs, staff indicated members are typically excited when they reach a live person rather than an automated call center, and this has had a positive impact on their ability to build trust with members.
Accurate Information Drives Better Outcomes
- Accurate Information Improves Access: In comparison to state Medicaid eligibility files that may have outdated information, the real-time availability of up-to-date, accurate contact information (e.g. phone number) within the Unite Us platform directly impacts the ability to successfully connect with members and supports other outreach initiatives by CTDHP.
Tailored Outreach Improves Member Reach and Engagement
- Unite Us Drives Increased Oral Health Referrals: CTDHP staff reported that since the implementation of Unite Us, their volume of member referrals for oral health services has significantly increased compared with their volume prior to Unite Us.
- Warm-Touch Outreach Enhances Member Engagement: Unlike automated reminder calls, which direct members without a recent dental health utilization claim to contact CTDHP, the Unite Us referral system supports CTDHP’s hands-on approach, reducing member burden.

“Those conversations are actually built into our initial assessment… We try to build [a] rapport with them so that they feel comfortable telling us what they need.”
Focus Group Member, Oral Health Navigator
Looking Forward
 To enhance the impact of the program, CTDHP is exploring the development of targeted referral pathways to better identify and connect members who would most benefit from social care coordination and dental navigation services. Key populations include:
To enhance the impact of the program, CTDHP is exploring the development of targeted referral pathways to better identify and connect members who would most benefit from social care coordination and dental navigation services. Key populations include:
- Pregnant individuals facing unique oral health needs linked to maternal and infant health outcomes.
- Members with acute dental needs who require timely intervention to prevent escalation.
- Members with low health literacy, intellectual or developmental disabilities (IDD), or complex care needs who may encounter significant barriers to accessing dental care and navigating the healthcare system.
Acknowledgments
This work would not be possible without the staff and leaders from CTDHP, who work tirelessly to support members across CT. We also express gratitude to the team members who contributed their time, expertise, and honest insights to support the creation of this case study. For additional information about CTDHP’s impact, visit https://ctdhp.org/reports/.
About Unite Us
Unite Us is the nation’s leading software company bringing sectors together to improve the health and well-being of communities. We drive the collaboration to identify, deliver, and pay for services that impact whole-person health. Through Unite Us’ national network and software, community-based organizations, government agencies, and healthcare organizations are all connected to better collaborate to meet the needs of the individuals in their communities.






