3 Trends Shaping Health and Community Care in 2025
A look at what we discussed in Unite Us’ 2025 mid-year town hall: from current market trends in community-based care to the customer stories driving us forward.
Last month, we hosted our biannual Customer Town Hall to connect directly with our customers and collaborate directly on the future of health and community care.
Together with our customers, we’re driving meaningful care coordination across the nation, bringing critical dollars back into communities, reducing administrative burden, and making a real difference in the lives of those we serve. Here’s a snapshot of what we talked about.
3 Key Trends in Community Health Care
Unite Us founders kicked us off at the Town Hall, sharing insights on trends in healthcare and community care—while emphasizing Unite Us’ role as a trusted partner for communities facing complex challenges.
We highlighted how technology continues to be a “force multiplier” for better service delivery, funding efficiency and data-driven insights across government, healthcare, payers, and community-based organizations.
Key Takeaways:
![]() Unite Us is integrating real-time eligibility data from state Medicaid Management Information Systems (MMIS).
Unite Us is integrating real-time eligibility data from state Medicaid Management Information Systems (MMIS).
![]() New capabilities support self-screening and data centralization across systems, reducing duplication and speeding up triage.
New capabilities support self-screening and data centralization across systems, reducing duplication and speeding up triage.
![]() AI is being integrated across the platform, from conversational screening to natural language queries for reporting.
AI is being integrated across the platform, from conversational screening to natural language queries for reporting.
Customers, governments, and funders all want to prove the value of their work. We emphasized Unite Us’ shared responsibility to help customers demonstrate outcomes, efficiencies, and cost savings.
Key Takeaways:
![]() Unite Us has a dedicated Research & Evaluation Team available to conduct ROI, utilization, and efficiency studies with customers.
Unite Us has a dedicated Research & Evaluation Team available to conduct ROI, utilization, and efficiency studies with customers.
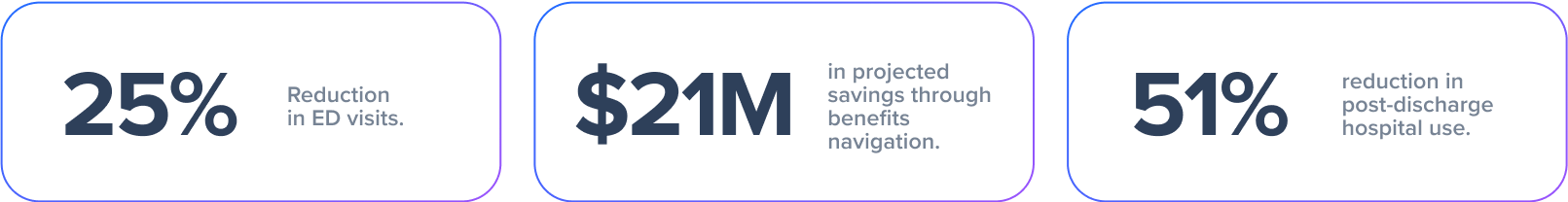
![]() Case studies from Ballad Health, Summit County, Ohio, and Bayhealth showed real results, including:
Case studies from Ballad Health, Summit County, Ohio, and Bayhealth showed real results, including:
We introduced Unite Us’ evolving predictive analytics tool, which focuses on identifying individuals at risk before a crisis occurs.
Key Takeaways:
![]() The model helps organizations understand which of the clients they serve may have non-medical needs (food insecurity, loneliness) or a high likelihood of ED utilization.
The model helps organizations understand which of the clients they serve may have non-medical needs (food insecurity, loneliness) or a high likelihood of ED utilization.
![]() Organizations can now engage the right people in the right way (by text vs. phone) and at the right time.
Organizations can now engage the right people in the right way (by text vs. phone) and at the right time.
![]() The tool adjusts risk scores in real-time as users receive services through the platform.
The tool adjusts risk scores in real-time as users receive services through the platform.
Customer Spotlight: Rhode Island Office of Veterans Services (RI OVS)
 Through their partnership with Unite Us, the Rhode Island Office of Veterans Services (RI OVS) has transformed the way they connect Veterans, service members, and their families to critical resources—particularly transportation, which is one of the state’s most pressing barriers to care.
Through their partnership with Unite Us, the Rhode Island Office of Veterans Services (RI OVS) has transformed the way they connect Veterans, service members, and their families to critical resources—particularly transportation, which is one of the state’s most pressing barriers to care.
By leveraging Unite Us’ data-driven insights, RI OVS identified a widespread gap in access to transportation. In response, they launched a targeted program that provides Veterans with an average of 59 unlimited-use bus passes per month. With these passes, RI OVS is helping improve access to medical and legal appointments, employment opportunities, family engagement, and overall well-being.
“Through the Unite Us platform and ‘No Wrong Door’ approach, we’ve built lasting, trusted partnerships that deliver real outcomes—and fast.”
—Jacques Deckstrader, RI Office of Veterans Services
Unite Us’ platform serves as the backbone of RI OVS’s coordination efforts. All requests, whether submitted through their website or by walk-in, are routed into a centralized coordination center. There, the team triages cases to the most appropriate community partner, reducing time to service and improving closure rates.
Key Outcomes:
- Average of 59+ unlimited bus passes issued monthly to support veterans’ independence.
- Seamless referral routing and high partner acceptance rates.
- Clear visibility into past services and provider history to inform care.
- Stronger trust and sustained relationships across Rhode Island’s veteran-serving network.
Customer Spotlight: AllCare Health
AllCare Health , a Coordinated Care Organization serving more than 65,000 Medicaid members in Southern Oregon, shared how they use Unite Us to improve care coordination across four rural counties.
, a Coordinated Care Organization serving more than 65,000 Medicaid members in Southern Oregon, shared how they use Unite Us to improve care coordination across four rural counties.
AllCare needed a coordinated approach to address not just medical care, but also crucial non-medical needs. By implementing the Unite Us platform across all 36 counties in Oregon, AllCare Health has transformed its care coordination capabilities. The decision was driven by the platform’s robust security, nationwide reach, and ability to embed state-mandated screening tools.
This “no-wrong-door” approach has created greater efficiency, provides clean data for state reporting, and fosters a more trauma-informed system where resources come directly to the member.
Key Outcomes:
- Launched in all 36 counties across Oregon
- 5,000 members served via Unite Us
- 387 community organizations onboarded
- Seamless referrals to services like transportation, housing, and behavioral health support.