Lighting the ToRCH: Powering Rural Health Transformation through a Hospital-Led Hub Approach
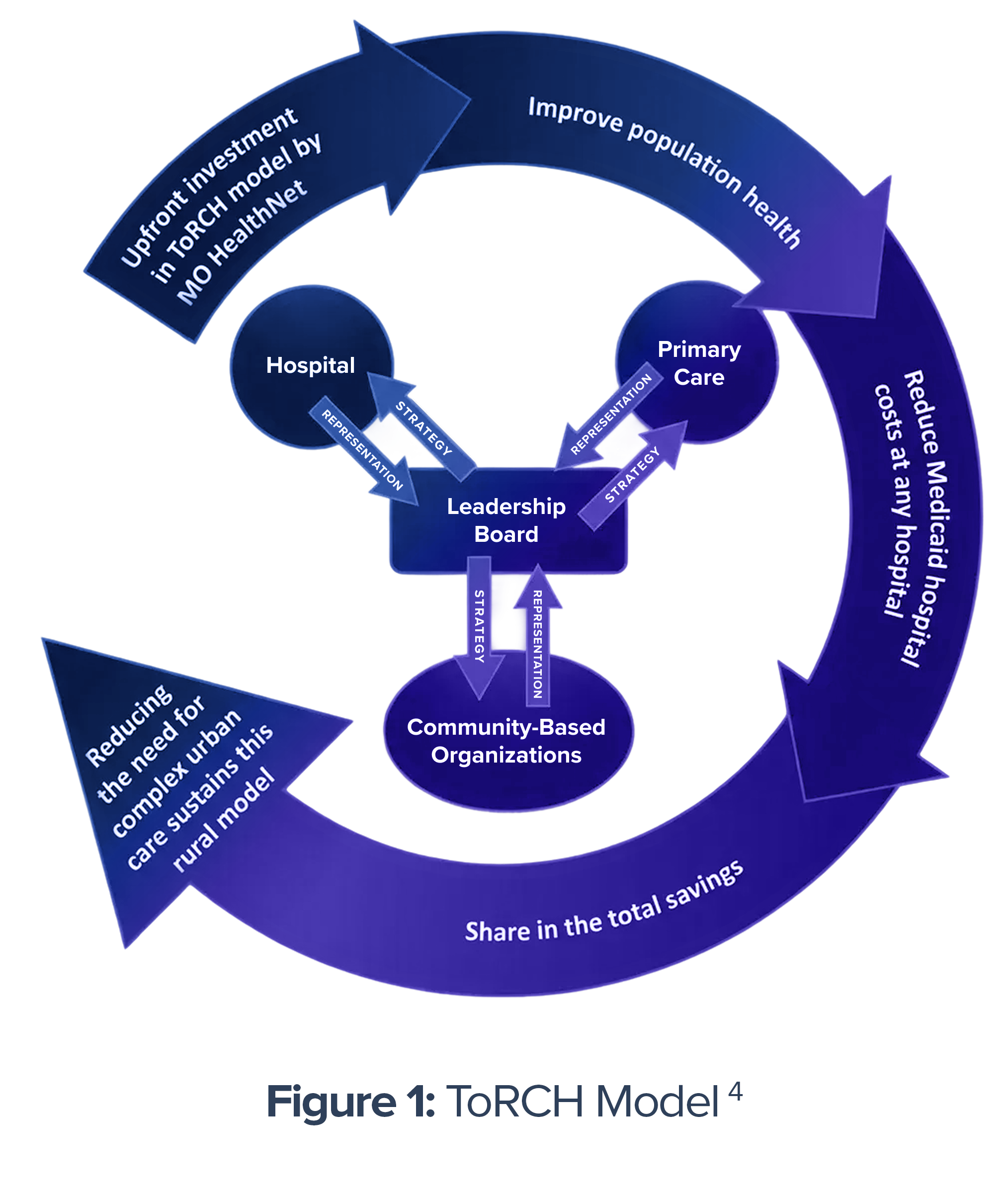
Missouri’s Transformation of Rural Community Health (ToRCH) program provides rural communities with the infrastructure and network they need to successfully coordinate care. Through Unite Us’ closed-loop referral system, participating providers can connect patients to community resources, streamline reimbursement, improve health outcomes, and minimize costs.
.
The Background: Laying the Groundwork for Integrated Rural Care
 The Transformation of Rural Community Health (ToRCH) program—supported by Missouri Medicaid—channels critical resources into rural communities to address the underlying social and economic factors that contribute to poor health outcomes. By embedding community-based care services within traditional clinical workflows, ToRCH strives to improve patient wellbeing, strengthen the financial sustainability of rural hospitals, and enhance chronic condition management. ToRCH focuses on optimizing existing funding streams while creating lasting, community-centered models of care in a fiscally responsible manner.
The Transformation of Rural Community Health (ToRCH) program—supported by Missouri Medicaid—channels critical resources into rural communities to address the underlying social and economic factors that contribute to poor health outcomes. By embedding community-based care services within traditional clinical workflows, ToRCH strives to improve patient wellbeing, strengthen the financial sustainability of rural hospitals, and enhance chronic condition management. ToRCH focuses on optimizing existing funding streams while creating lasting, community-centered models of care in a fiscally responsible manner.
The Challenge: Closing Critical Gaps in Rural Health
The Rural Health Transformation Program¹ offers a timely opportunity to tackle challenges unique to rural America. Rural communities face limited access to care due to distance, transportation barriers, and provider shortages² —alongside higher rates of poverty and fewer economic opportunities³. These factors heighten vulnerability to non-medical drivers of health, such as food, housing, and transportation insecurity, which can worsen health outcomes. But at the same time, rural communities possess unique strengths: they often have a strong sense of community and a resilient mindset. By partnering with community organizations, rural providers can leverage these strengths to help address health-related needs and improve population health, backed by secure data-sharing technology infrastructure.

“We haven’t wrapped our arms around them [patients/community members] like this. We haven’t done our job. Through ToRCH we’re getting them back on their feet.”
Marvin Smoot, VP of Clinical Operations, Bothwell Regional Health Care Center
The Solution: A Unite Us-Powered Model for Rural Transformation
Missouri’s ToRCH initiative—funded through a unique application of the 1915(b) waiver authority—was designed to directly confront the interconnected challenges of rural health.
With Unite Us as the technology backbone, hospitals connect seamlessly with community-based organizations through a Community Information Exchange (CIE) that enables secure, closed-loop referrals and Medicaid reimbursement for certain care services delivered.
Since July 2024, six participating hospitals have acted as ToRCH Hub leads. These hub leads serve as central access points for coordinated care across their communities and are incentivized through outcome-based payments beginning in 2026 and shared savings beginning in 2028.
How It Works
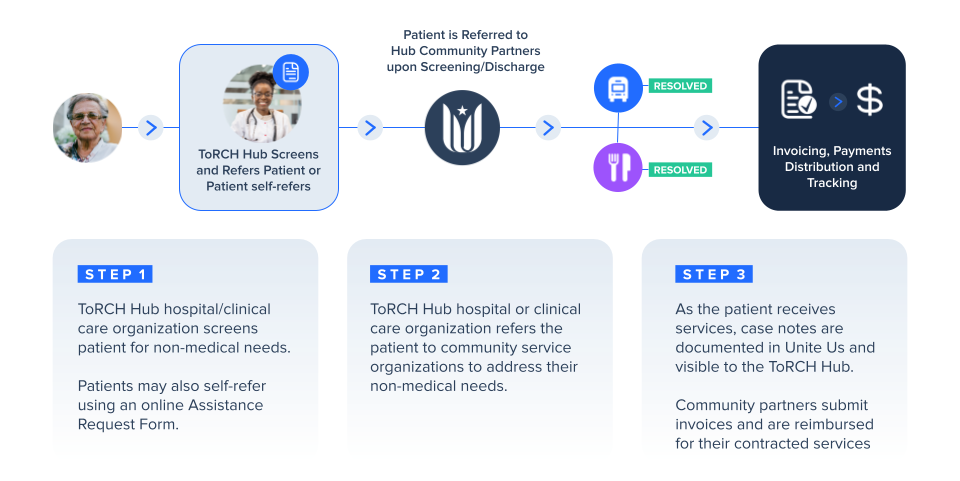
Through Unite Us’ closed-loop referral platform, clinical staff at participating organizations within ToRCH Hubs refer patients to community-based organizations to address their non-medical needs. The ToRCH model of care not only enables patients to access both the health and community care they need, but also reimburses community service organizations addressing transportation, food assistance, home modifications, and environmental services when documented as a health-related need.
The Impact: Technology-Driven Transformation in Rural Missouri
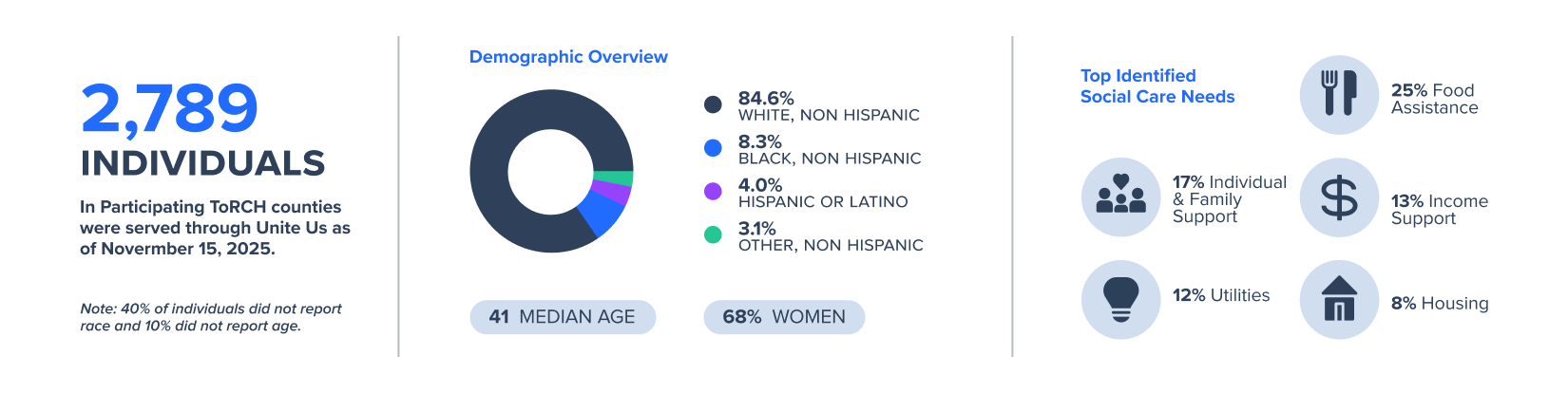
Across the six participating Missouri ToRCH counties—Dent, Henry, Pettis, Phelps, Polk, and Ray— referrals have been sent on behalf of 2,789 individuals for over 900 community services,⁵ with 66% of all referral activity initiated by ToRCH Hubs.

“Prior to ToRCH, we did not have consistent case management efforts. This model has enabled us to put social risk screenings in place and a way in which to follow up on them.”
Tabitha Stanfast, BSN, RN, LSSYB, Salem Memorial Hospital
ToRCH Hub Results
ToRCH demonstrated that locally governed, data-driven collaboration can improve both outcomes and financial stability. Participating hospitals and clinics achieved measurable results, including a 19.6% increase in individuals with controlled blood pressure and an 18% increase in behavioral-health follow-up after ED visits. These are critical Healthcare Effectiveness Data and Information Set (HEDIS) measures, given evidence suggests that patients who fail to receive aftercare following their emergency psychiatric visit have 6 times higher odds of returning to the ED within 2 months.⁶ Similarly, a person with hypertension is four times more likely to die from a stroke and three times more likely to die from heart disease if no after-care is received.⁷
Mean increase in rate of patients with a controlled blood pressure ICD-10 code across participating ToRCH Hubs and clinics.
Mean improvement in behavioral health follow-ups after an ED visit, a critical National Committee for Quality Assurance (NCQA) quality measure, across participating ToRCH Hubs and clinics.
From 9/3/2024 - 11/15/2025, 99% of all CBO invoices were accepted and paid within 90 days, compared to medical billing 5-10% claims denial industry benchmark.
Figure 4: ToRCH Impact to Date (Jun 2023-Nov 2025)
.
Satisfaction with ToRCH Model
ToRCH Hub end users were invited to participate in a cross-sectional survey capturing feedback and satisfaction with Unite Us’ platform as well as impact on administrative efficiency. In addition to the findings noted in figure 5, 88% of respondents agreed the ToRCH model improves overall patient care, and a majority of respondents reported feeling less stressed about documenting outcomes and follow up on patient referrals since using Unite Us.
Average time savings reported by ToRCH Hub end users (n=33) via a cross-sectional survey (September, 2025). This represents 1,067 administrative hours gained and approximately $26,675 in salary savings.
Of surveyed HUB end users (n=33), 92% report the ToRCH model and shared incentives were key to improving community care coordination.
Of surveyed HUB end users (n=33), 100% report they are confident in their ability to connect patients with community resources to meet their non-medical needs.
Figure 5: ToRCH Workforce Impact to Date (Jun 2023 – Nov 2025)
.
Compliance and Administrative Efficiency Gains
Unite Us’ platform capabilities also allow the Medicaid program to meet federal requirements under the waiver. The grant tracking and reimbursement module strengthens accountability by clearly demonstrating that payments are made only for services authorized in the waiver language. This transparency streamlines administrative oversight, reduces compliance risk, and helps ensure the program secures the full federal matching funds for which it is eligible.
“For the first time in my Social Work career, I finally feel like I’m truly making a difference in people’s lives!”
–ToRCH Hub Social Worker
“It functions perfectly when referrals receive prompt responses and are accepted. Leaves me feeling good with less stress to know they are getting the help needed.”
–Resources Specialist/Social Worker
In addition to those critical reporting capabilities, ToRCH end users reported an average of 17 minutes in time saved per referred case, translating to $27K in administrative cost savings alone.
Partner Spotlight: Bothwell Regional Health Center
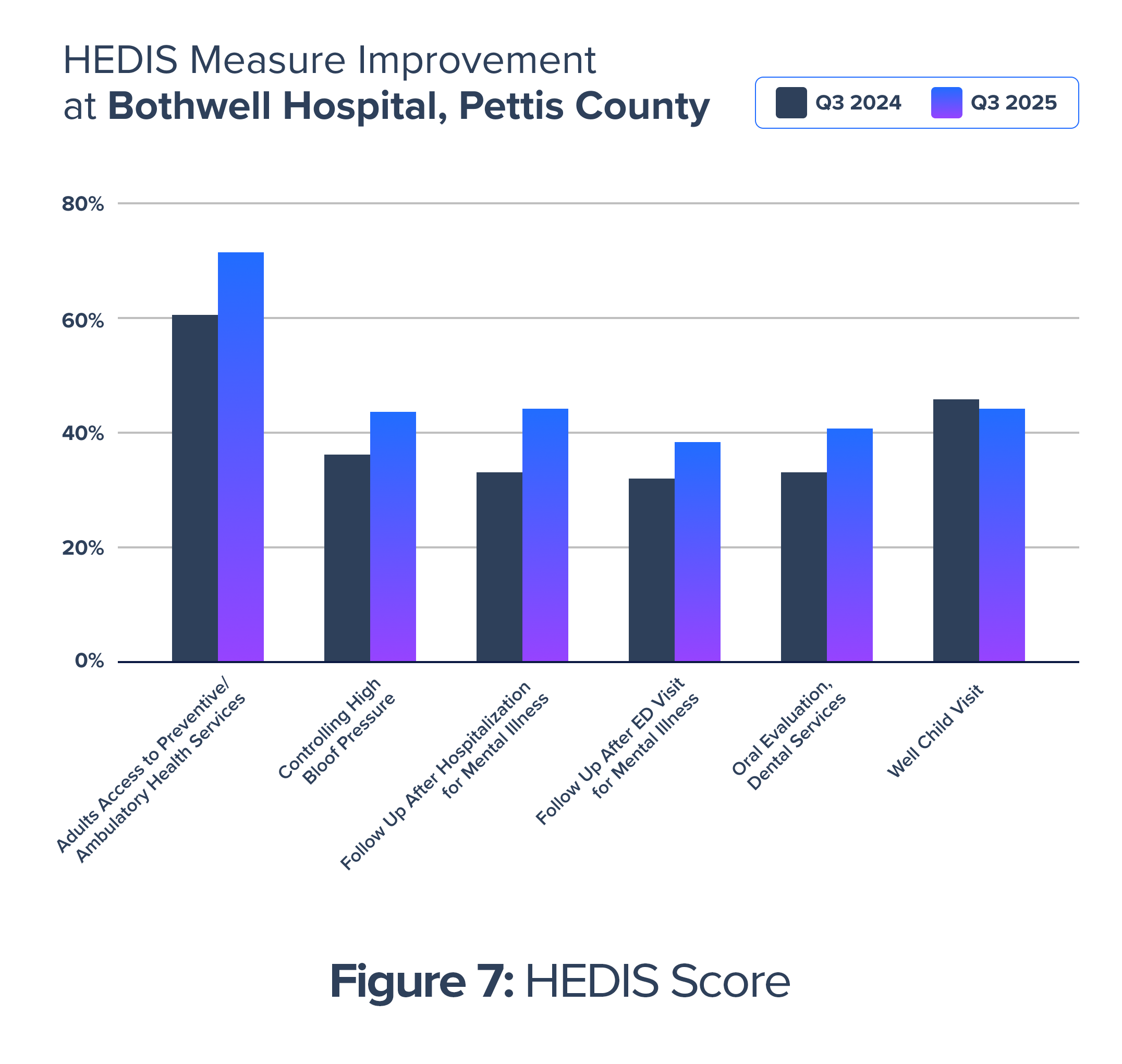 As one of the six ToRCH hub leads, Bothwell Regional Health Center demonstrates how technology-enabled collaboration can move the needle on key metrics.⁸
As one of the six ToRCH hub leads, Bothwell Regional Health Center demonstrates how technology-enabled collaboration can move the needle on key metrics.⁸
A recent study conducted by the Veterans Health Administration found that each additional in-person primary care visit was associated with a cost reduction of $721 per person per year.⁹ Applied to the 10% increase from Q3 2024 to Q3 2025 in Bothwell patients with Adults’ Access to Ambulatory/Preventive Health Services (AAP) Gap Closure, this represents an estimated $381K in reduced annual healthcare costs, for that measure alone.

Real People, Real Impact
The ToRCH model’s primary objective is to proactively improve patient outcomes by addressing non-medical needs through examples like the following:
“I had a 32-year-old Army veteran who had been recently medically discharged. He was on the verge of losing his home because he was paying outrageous utility bills. He hadn’t had heating/cooling in his home for 2 years and was using 6 space heaters during the winter and 3-4 A/C window units during the summer. He had also been seen in our ER 49 times for COPD, pneumonia, etc within a year. We were able to get him a brand-new heating/cooling unit. His bills have become more manageable, and he has not been seen in our ER since he got the new unit and his children’s outcomes improved.”
ToRCH Social Worker
Lessons Learned: A Blueprint for Rural Health Innovation
The ToRCH pilot demonstrates that a community-led, hospital-anchored care model can be both effective and scalable in rural areas. Leveraging cross-sector collaboration and digital infrastructure, ToRCH increases access to social support while improving overall patient care and well-being. High referral resolution, efficient processes, and the integration of CBOs into care workflows signal strong potential for replicability and broader system impact, particularly in the rural health care setting. The findings reinforce the role of rural hospitals as care coordination leaders capable of advancing population health through strategic partnerships and data-driven strategies.

Implications for Practice
- Hospital Leadership: Rural hospitals can serve as central coordinators of health and community-based care when supported by targeted funding and outcome-based incentives. This leadership model supports more holistic care delivery and can be adapted in similar rural settings.
- Cross-Sector Collaboration: The success of ToRCH highlights the importance of trust and coordination between clinical providers and community organizations. Strong, sustained partnerships are essential to meeting complex patient needs.
- Technology as a Connector: Tools like Unite Us facilitate seamless, secure communication between partners and help track patient progress across systems. Investment in such platforms is crucial for efficient and accountable care coordination.
- Incentive Alignment: ToRCH’s shared savings approach encourages measurable improvements in care outcomes and reduces avoidable hospital utilization, offering a blueprint for Medicaid programs seeking to align payment with value.
- Data-Driven Improvement: Ongoing evaluation and use of referral and utilization data enable continuous refinement of the model. This real-time feedback is key to scaling ToRCH and sustaining impact over time.

“Be willing to try anything and if it doesn’t succeed, don’t label it a failure. Bring people to your table that don’t agree with you or your point of view – they likely see another perspective that can be easily missed.”
Tabitha Stanfast, BSN, RN, LSSYB, Salem Memorial Hospital
Conclusion: Unite Us—Your Partner in Rural Health Transformation

The ToRCH model is more than a pilot—it demonstrates what’s possible when technology, partnership, and purpose unite.
With Unite Us as the trusted infrastructure partner, states and health systems can build sustainable, connected ecosystems that meet both health and non-medical needs—delivering measurable value for patients, providers, and communities.
Together, we’re building the future of rural health—one referral, one relationship, and one resilient community at a time.
Explore Our Rural Health Solutions
About Unite Us
Unite Us is the nation’s leading software company bringing sectors together to improve the health and well-being of communities. We drive the collaboration to identify, deliver, and pay for services that impact whole-person health. Through Unite Us’ national network and software, community-based organizations, government agencies, and healthcare organizations are all connected to better collaborate to meet the needs of the individuals in their communities.