Transforming Social Care Payments with Automated Medicaid Member Eligibility Verification
By: Emily Anders, Director, Payment StrategyHow automating the member eligibility verification process in real-time accelerates reimbursements and improves access to social care services.
More than 77 million Americans rely on Medicaid for health insurance.
Yet enrolling individuals in Medicaid programs, connecting them to care, and facilitating payments for services can be challenging for organizations responsible for delivering these services.
With more states such as New York and Oregon harnessing their states’ Medicaid 1115 waivers to pilot projects designed to better serve Medicaid members and address health-related social needs (HRSN), streamlining Medicaid enrollment, authorization, and reimbursement processes is becoming increasingly imperative for expanding access to critical social care services.
As more government agencies, health plans, providers, and community-based organizations (CBOs) engage in cross-sector initiatives aimed at advancing social care outcomes, doing this work efficiently, and at scale, is more important than ever.
Challenges with Traditional Member Eligibility Verification and How Unite Us Is Solving Them
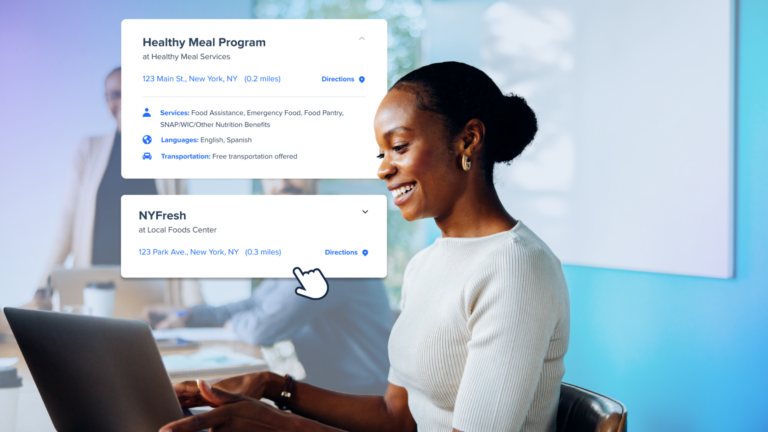
Member eligibility verification is typically a time-intensive, cumbersome process, with care managers manually toggling between multiple systems to verify member eligibility and connect them to a CBO’s services. Not only is this frustrating for staff, but it also means delays and bottlenecks for Medicaid members who need to be connected to vital resources. Without technology that helps care managers accelerate this process and centralize social care coordination, resources are wasted and staff is placed under intense administrative burden.
Unite Us is solving this problem by integrating with states’ Medicaid systems in real-time, eliminating the need to access multiple systems and reducing the administrative burden of manually verifying Medicaid eligibility and managed care enrollment each time services are needed. This integration enhances the Medicaid reimbursement process by seamlessly incorporating real-time verification into the workflow of Unite Us’ scalable payments solution, streamlining and automating a traditionally tedious process.
How does it work? First, a user adds insurance information to a member’s profile. Unite Us automatically sends a request to a state Medicaid system to verify the member’s insurance coverage with the selected plan. Users are notified if the member is eligible to be enrolled in the social care program. The system also re-verifies member coverage to ensure continued program eligibility, as members often transition in and out of Medicaid or have lapses in their coverage.
With this functionality, care managers can seamlessly verify a member’s Medicaid coverage and eligibility for social care services with the click of a button, all within the Unite Us ecosystem.
Key Benefits of Automated Member Eligibility Verification
The ability to seamlessly integrate with states’ Medicaid systems in real time holds several advantages, including:
- Enable automation to increase efficiency for care managers – The ability to automatically verify a member’s eligibility for Medicaid insurance empowers care teams to provide high-quality care. Closer integration between health care and social care results in increased efficiencies and faster case resolutions.
- Build a scalable infrastructure for social care funding – Integrations between social care technology platforms and claims processing platforms are critical in creating a secure, connected ecosystem that enables care managers to do their jobs at scale.
- Improve health outcomes while decreasing billing denials – Here’s the bottom line: if health plans are able to accurately confirm that a member is eligible to receive social care services before those services are delivered, then members’ health outcomes improve and billing denials decrease, which ensures that CBOs get reimbursed in a timely manner and can scale their service offering.
- Protect against fraud, waste, and abuse: Care teams can easily see if a member needs to be disenrolled from a billable program if they’re no longer eligible to receive services.
Customer Success Story: NCDHHS
The Healthy Opportunities Pilot (HOP), North Carolina’s 1115 HRSN Medicaid demonstration waiver, authorized the reimbursement of $650 million for health-related social need (HRSN) services to Medicaid members.
This program by the North Carolina Department of Health and Human Services (NCDHHS) is the nation’s first comprehensive program to provide evidence-based interventions—including housing, food, transportation, interpersonal safety, and toxic stress support services—to high-needs Medicaid enrollees.
Working in partnership with NCDHHS, Unite Us recently launched an integration with North Carolina’s MMIS system to streamline real-time member eligibility verification.
Since the HOP program launched in March 2022, there has been an incredible impact with invoice metrics citing a 3% payer rejection rate1 compared to the national denials rate of 18%2 – and more than $70M has been reimbursed for health-related social needs services as of April 30, 2024.3
- Unite Us data collected from 03/15/22-10/03/23
- The Change Healthcare 2020 Revenue Cycle Denials Index
- NC Department of Health and Human Services data
How Does this Simplify Reimbursement for Social Care?
Integrating real-time member eligibility verification into social care technology is a significant step forward in the larger ecosystem of social care reimbursement programs. Now more than ever, closer interoperability between healthcare and social care technology systems results in increased efficiencies, empowering government, healthcare, and community organizations to support Medicaid populations in a more sustainable, scalable way. Pulling these various stakeholders together is a critical piece of doing this work at scale.
Now, insurance verification and program enrollment can happen all in one system, allowing these organizations to collaborate and support Medicaid populations in a way they haven’t been able to before.
- CBOs: Use one simple tool to confirm that individuals are eligible to receive services before they walk in the door, and access sustainable funding while serving the greatest number of people possible.
- Health Plans: Verify member’s eligibility for social care programs with one efficient, accurate system. Easily reimburse CBOs for services provided and ensure that claims are being sent to the right place while enabling cross-sector care teams to seamlessly identify any coverage gaps and get a member re-enrolled in services.
- Government: Verify constituent’s eligibility for social care programs with one efficient, accurate system. Utilize one technology across Medicaid systems to address a population’s SDoH needs at scale and ensure that no one is falling through cracks in the system.
- Providers: When submitting referrals for patients, quickly see at the point of care if they are eligible for services, and access streamlined support in the community.
While this work can be complex, the goal is simple: making sure that Medicaid members are receiving the benefits they’re eligible for as efficiently as possible. Real-time member eligibility verification represents an important first step in this journey and makes it clear that there’s an opportunity for all organizations, no matter how small, to shape the future of social care payments and build healthier, more resilient communities.
To learn more about Unite Us Payments